Comparison of Pioglitazone vs. Glimepiride on Progression of Coronary Atherosclerosis in Patients With Type 2 Diabetes
Comparison of Pioglitazone vs. Glimepiride on Progression of Coronary Atherosclerosis in Patients With Type 2 Diabetes
Comparison of Pioglitazone vs. Glimepiride on Progression of Coronary Atherosclerosis in Patients With Type 2 Diabetes
2008-04-09
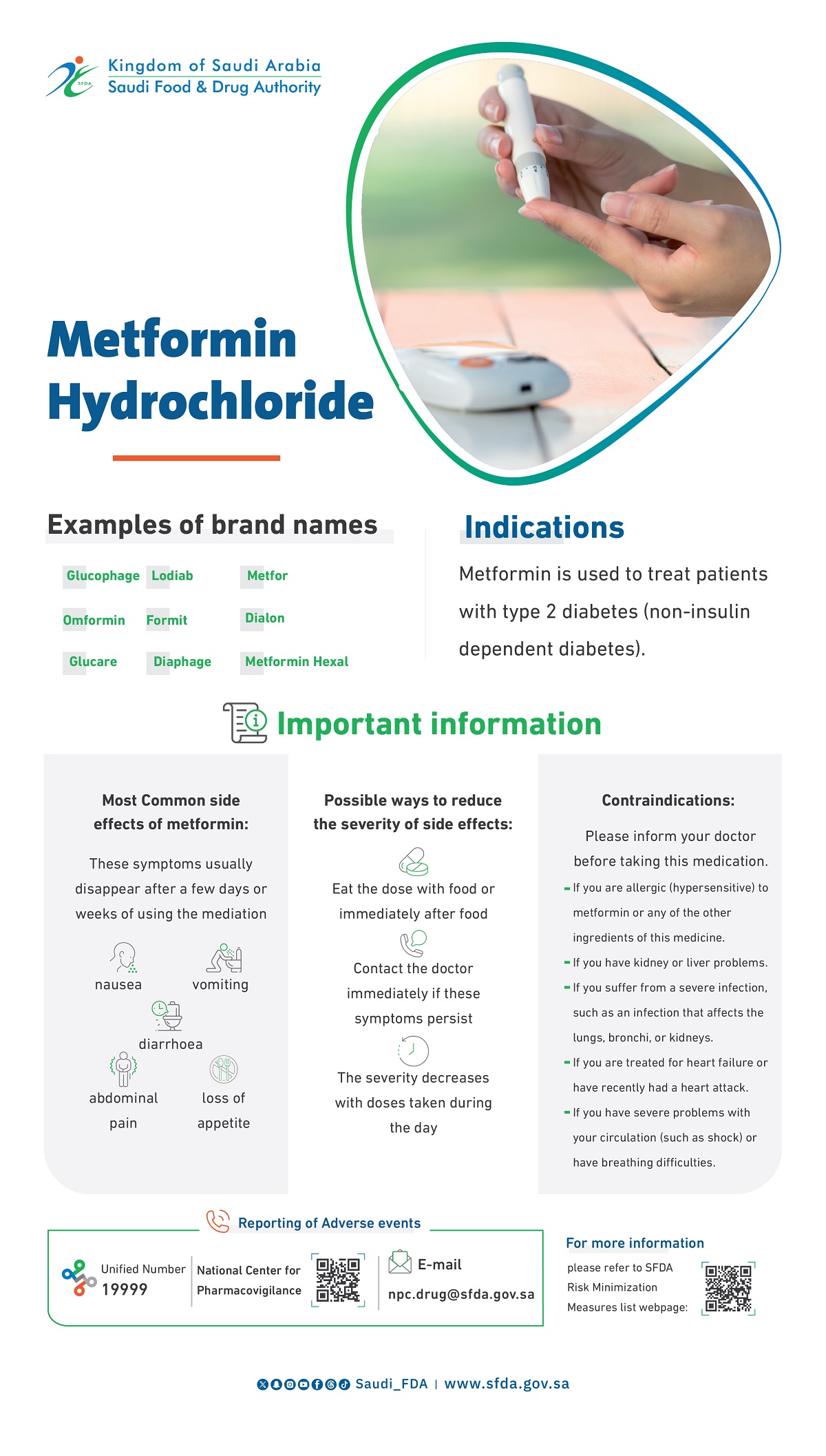
No antidiabetic regimen has demonstrated the ability to reduce progression of coronary atherosclerosis. Commonly used oral glucose-lowering agents include sulfonylureas, which are insulin secretagogues, and thiazolidinediones, which are insulin sensitizers.
The objectives of the study were to compare the effects of an insulin sensitizer, Pioglitazone, with an insulin secretagogue, Glimepiride, on the progression of coronary atherosclerosis in patients with type 2 diabetes.
The study was a double-blind, randomized, multicenter trial at 97 academic and community hospitals in North and South America (enrollment August 2003-March 2006) in 543 patients with coronary disease and type 2 diabetes. A total of 543 patients underwent coronary intravascular ultrasonography and were randomized to receive Glimepiride, 1 to 4 mg, or Pioglitazone, 15 to 45 mg, for 18 months with titration to maximum dosage, if tolerated. Atherosclerosis progression was measured by repeat intravascular ultrasonography examination in 360 patients at study completion.
Least squares mean PAV increased 0.73% (95% CI, 0.33% to 1.12%) with Glimepiride and decreased 0.16% (95% CI, –0.57% to 0.25%) with Pioglitazone (P = .002). An alternative analysis imputing values for noncompleters based on baseline characteristics showed an increase in PAV of 0.64% (95% CI, 0.23% to 1.05%) for Glimepiride and a decrease of 0.06% (–0.47% to 0.35%) for Pioglitazone (between-group P = .02).
Mean (SD) baseline HbA1c levels were 7.4% (1.0%) in both groups and declined during treatment an average 0.55% (95% CI, –0.68% to –0.42%) with Pioglitazone and 0.36% (95% CI, –0.48% to –0.24%) with Glimepiride (between-group P = .03). In the Pioglitazone group, compared with Glimepiride, high-density lipoprotein levels increased 5.7 mg/dL (95% CI, 4.4 to 7.0 mg/dL; 16.0%) vs 0.9 mg/dL (95% CI, –0.3 to 2.1 mg/dL; 4.1%), and median triglyceride levels decreased 16.3 mg/dL (95% CI, –27.7 to –11.0 mg/dL; 15.3%) vs an increase of 3.3 mg/dL (95% CI, –10.7 to 11.7 mg/dL; 0.6%) (P < .001 for both comparisons).
Median fasting insulin levels decreased with Pioglitazone and increased with Glimepiride (P < .001). Hypoglycemia was more common in the Glimepiride group and edema, fractures, and decreased hemoglobin levels occurred more frequently in the Pioglitazone group.
In patients with type 2 diabetes and coronary artery disease, treatment with Pioglitazone resulted in a significantly lower rate of progression of coronary atherosclerosis compared with Glimepiride.
Source: JAMA. 2008;299(13):1561-1573