Arsenic Exposure and Prevalence of Type 2 Diabetes in US Adults
Arsenic Exposure and Prevalence of Type 2 Diabetes in US Adults
Arsenic Exposure and Prevalence of Type 2 Diabetes in US Adults
2011-12-18
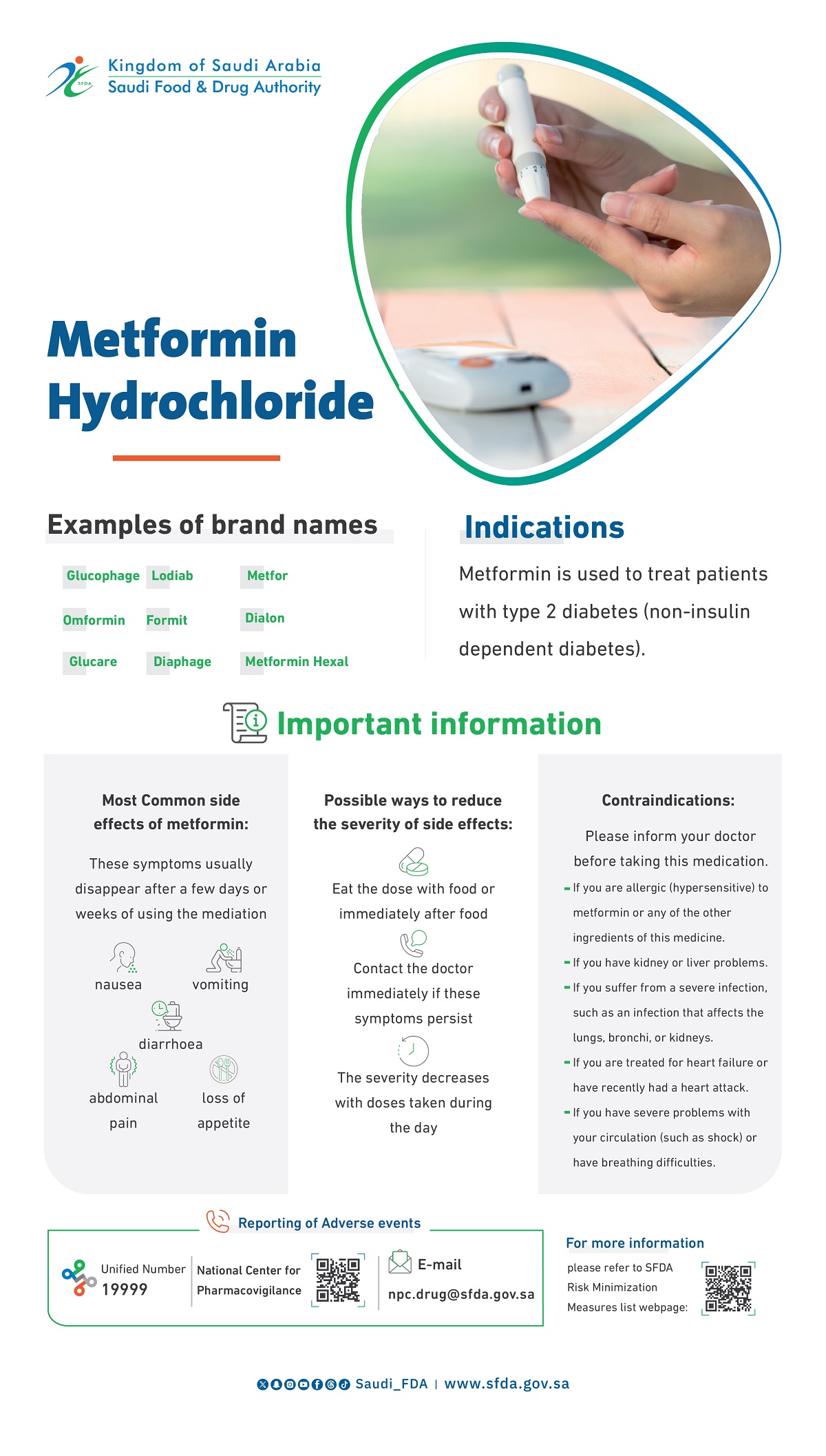
Context High chronic exposure to inorganic arsenic in drinking water has been related to diabetes development, but the effect of exposure to low to moderate levels of inorganic arsenic on diabetes risk is unknown. In contrast, arsenobetaine, an organic arsenic compound derived from seafood intake, is considered nontoxic.
Objective To investigate the association of arsenic exposure, as measured in urine, with the prevalence of type 2 diabetes in a representative sample of US adults.
Design, Setting, and Participants Cross-sectional study in 788 adults aged 20 years or older who participated in the 2003-2004 National Health and Nutrition Examination Survey (NHANES) and had urine arsenic determinations.
Main Outcome Measure Prevalence of type 2 diabetes across intake of arsenic.
Results The median urine levels of total arsenic, dimethylarsinate, and arsenobetaine were 7.1, 3.0, and 0.9 µg/L, respectively. The prevalence of type 2 diabetes was 7.7%. After adjustment for diabetes risk factors and markers of seafood intake, participants with type 2 diabetes had a 26% higher level of total arsenic (95% confidence interval [CI], 2.0%-56.0%) and a nonsignificant 10% higher level of dimethylarsinate (95% CI, –8.0% to 33.0%) than participants without type 2 diabetes, and levels of arsenobetaine were similar to those of participants without type 2 diabetes. After similar adjustment, the odds ratios for type 2 diabetes comparing participants at the 80th vs the 20th percentiles were 3.58 for the level of total arsenic (95% CI, 1.18-10.83), 1.57 for dimethylarsinate (95% CI, 0.89-2.76), and 0.69 for arsenobetaine (95% CI, 0.33-1.48).
Conclusions After adjustment for biomarkers of seafood intake, total urine arsenic was associated with increased prevalence of type 2 diabetes. This finding supports the hypothesis that low levels of exposure to inorganic arsenic in drinking water, a widespread exposure worldwide, may play a role in diabetes prevalence. Prospective studies in populations exposed to a range of inorganic arsenic levels are needed to establish whether this association is causal.
JAMA. 2008;300(7):814-822